
Some Indiana doctors are raising fears about possible loss of emergency services under a plan to limit “surprise” medical bills.
FILE PHOTO: Lauren Chapman/IPB NewsINDIANAPOLIS (AP) — Some Indiana doctors are raising fears about possible loss of emergency services under a plan to limit “surprise” medical bills that can plague patients who have been unknowingly treated by providers from outside their insurance networks.
The proposed state law is a top priority of House and Senate leaders in the Republican-dominated Legislature who see it as a step toward reigning in health care costs. Major business groups and health insurers are supporting the plan as lawmakers work to reach a deal in the final weeks of this year’s legislative session.
Key provisions of the bill would prohibit medical providers from charging higher out-of-network rates to a patient who was treated a facility that was within their health insurance network unless that patient agreed in advance to pay the higher cost.
Many surprise bills, however, stem from emergencies where a patient can wind up at a hospital that’s not in their insurer’s network. Even at an in-network hospital, emergency physicians or anesthesiologists are often not hospital employees and may not have a contract with the patient’s insurance company.
Some doctors maintain the Indiana proposal gives all the power to insurance companies on what to pay so that they have no incentive to negotiate contracts with the doctors. The Indiana State Medical Association, which represents physicians across the state, warns that will lead to lower payments and possibly leave more rural hospitals without enough emergency doctors as the number of physician groups shrink.
Most hospitals across the state have contracts with independent doctor groups to provide emergency room staffing, said Dr. Christian Ross, a partner in a group of about 40 physicians that covers emergency departments at four Community Health Network hospitals in Indianapolis and one in Kokomo.
The state proposal would essentially allow insurers to pay whatever rate they wanted to emergency doctors, Ross said.
“For small groups like us, it’s going to more or less cripple us,” he said. “We wouldn’t be able to continue to hire positions in Indiana. We wouldn’t be able to retain what physicians we have because we wouldn’t be able to negotiate appropriately with the payers, so we wouldn’t be able to maintain salaries here.”
The doctors support establishing a system of independent arbitration aimed at resolving disputes over surprise bills, which has bipartisan backing in Congress and from the Trump administration.
Indiana business groups and insurance companies argue such arbitration systems have increased costs in other states.
“We think there are problems in the (arbitration) scenario and that would be our line in the sand,” Mike Ripley, the Indiana Chamber of Commerce’s vice president for health care, said during a recent hearing on the bill.
State Rep. Ben Smaltz, the surprise billing measure’s sponsor, said he had not seen evidence that the proposal would cause doctors to leave the state and that he was more concerned about people not seeking needed treatment after being hit by such medical bills.
“The money side will resolve itself somehow,” said Smaltz, a Republican from Auburn. “I’m trying to solve it for the taxpayer, the patient, the individual. I’m trying to help them. They’re not the ones who created this system; they’re the victims of it.”
The legislation also faces questions over how many people it could actually cover as many employer-provided health insurance plans are regulated by federal law. The state medical association estimates that perhaps only 15% of Indiana insurance plans could fall under the state law.
State Senate President Pro Tem Rodric Bray, a Martinsville Republican, said steps toward greater health care cost transparency were important and that he was confident that lawmakers would reach an agreement before the legislative session ends in mid-March.
 DONATE
DONATE




 View More Articles
View More Articles


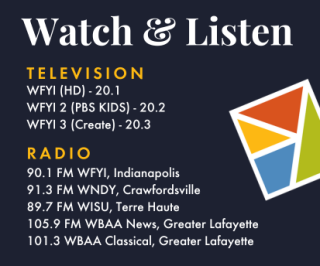

 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.