
Seema Verma is sworn in as the Centers for Medicare and Medicaid Services administrator.
Wikimedia Commons
Kentucky got the green light from the federal government Friday to require people who get Medicaid to work. It's a big change from the Obama administration, which rejected overtures from states that wanted to add a work requirement.
Medicaid's chief federal officer is Seema Verma; her home state of Indiana submitted plans for a work requirement last year, and the approval letter could come any day now. Under the proposal, people would have to average 20 hours a week of work or another qualifying activity — such as volunteering or getting an education — to get Medicaid.
The goal is to increase employment among Medicaid recipients. But Sara Rosenbaum, a professor of health law and policy at George Washington University, says there's a problem with that — most people on Medicaid are already working, or looking for work. Or they're caring for a child or family member, or they're sick or disabled.
Many of those people would be exempt from a work requirement, and states could also make some allowances for people battling addiction. When you consider all those exemptions, says Rosenbaum, "There is this very, very tiny slice of [of the population] who can work and simply choose not to work and apply for public assistance."
And even if states create programs that help people find jobs, and provide things like childcare and transportation, Rosenbaum says, there's no evidence that they would lead to more employment. And those programs are expensive.
"If you do a work program, it costs real money," she says, "and the federal government has said, 'we won't pay any of those costs.' "
What's more likely, Rosenbaum says, is that states will basically say, 'Get a job on your own, or get off Medicaid.' "
And what that does, she says, is create a hurdle for everybody on Medicaid. People who are working are going to have to prove they are employed, so even people with jobs could stand to lose their insurance because of red tape. In fact, the state of Indiana's own projections show that with a work requirement, Medicaid will cover fewer people and cost more.
Adam Mueller is an attorney at Indiana Legal Services, which helps people navigate that state's Medicaid program. He says people already lose coverage because the program can be confusing, and there are administrative errors.
"Somewhere along the way, paperwork gets lost; there's a miscommunication," he says, "Folks have sometimes had difficulty proving something as easy as residency."
And people on Medicaid often deal with crises – they may move a lot, or change phone numbers, which makes it hard to keep track of paperwork. Adding a work requirement on top of all that, Mueller says, would make staying enrolled even harder.
"There are a lot of things that can trip folks up, and that could lead to falling through the cracks," he says.
Judith Solomon, of the Center for Budget and Policy Priorities, points out that expanded Medicaid helps some employers, too.
"We have an economic structure where there are people whose employment doesn't provide health care," she says.
If employees lose Medicaid, get sick and can't make it to work, she says that's bad for business.
Verma told reporters during a conference call Thursday that the requirement is supposed to help people.
"People moving off of Medicaid is a good outcome," she said, "because we hope that that means they do not need the program anymore, that they have transitioned to a job that provides health insurance or that they can afford insurance on their own. This policy helps people achieve the American dream."
But advocates say the main purpose of Medicaid is to provide health insurance, not increase employment. And until now, the federal government agreed.
Susan Jo Thomas heads Covering Kids and Families of Indiana, which advocates for health coverage in the state. Under Medicaid's new management, she says, the philosophy surrounding work requirements has changed.
"I don't know if it jibes with my view of Medicaid, but my view of Medicaid now is irrelevant," she says. "It's what Seema Verma and the administration and the folks who are at CMS decide."
Thomas says she is taking more of a wait and see approach — the details of the work requirement have yet to be ironed out. She says if too many people lose insurance, she'll be raising concerns with the state.
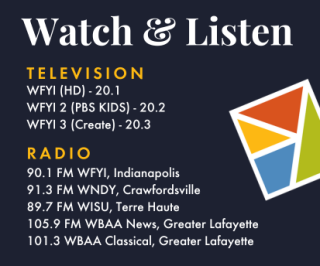
This story is part of NPR's reporting partnership with Side Effects Public Media, WFYI and Kaiser Health News.
 DONATE
DONATE






 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.