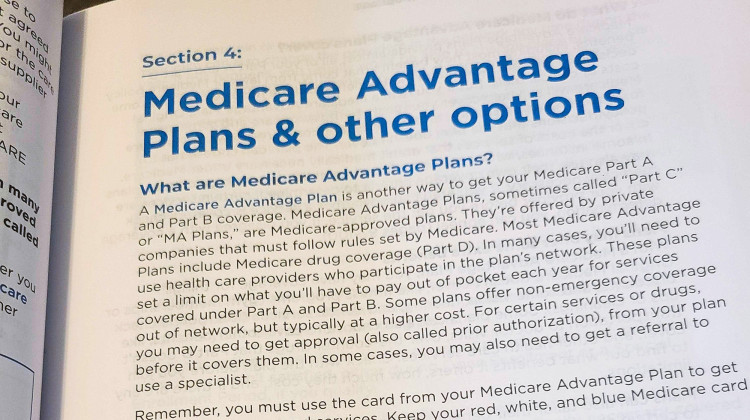
Medicare Advantage plans — sometimes called Part C plans — are administered by commercial insurers that follow rules set by the Centers for Medicare and Medicaid Services. President-elect Donald Trump’s pick to lead CMS has shown support for the growth of these private health plans, which would further privatize the program.
Kirsten Adair / IPB NewsRural health leaders are concerned about the potential growth of Medicare Advantage plans under the incoming Trump administration. The plans can exclude rural hospitals and clinics from provider networks – which creates unique problems for those communities.
Medicare Advantage plans — sometimes called Part C plans — are administered by commercial insurers that follow rules set by the Centers for Medicare and Medicaid Services. President-elect Donald Trump’s pick for the head of CMS has shown support for the growth of these private health plans, which would further privatize the program.
Brock Slabach, with the National Rural Health Association, said the growth of Medicare Advantage plans has posed problems for rural clinics and hospitals across the country.
“In Indiana, you can see that you've had a 60 percent increase—roughly 60 to 80 percent increase in the number of people that have chosen [Medicare Advantage] as a source for their insurance,” Slabach said.
Join the conversation and sign up for the Indiana Two-Way. Text "Indiana" to 765-275-1120. Your comments and questions in response to our weekly text help us find the answers you need on Medicaid and other statewide issues.
Slabach said people with these plans could lose coverage at rural facilities because insurers aren’t required to cover every willing provider. He said the plans just have to ensure access meets certain time and distance standards.
For example, plans have to ensure members in rural counties have access to a primary care provider or clinic within 40 miles and 30 minutes. In rural communities, members have to have access to a hospital within 75 minutes and 60 miles.
“We consider that to be offensive and we need to get some protections with some kind of any-willing-provider provision for these [Medicare Advantage] plans,” Slabach said.
The Indiana Rural Health Association also said addressing Medicare Advantage plans is one of its 2025 advocacy priorities.
Abigail is our health reporter. Contact them at aruhman@wboi.org.
 DONATE
DONATE








 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.