
Dr. Samuel Urrutia and his wife moved to the US in 2018 from Honduras to pursue his medical residency in internal medicine at IU.
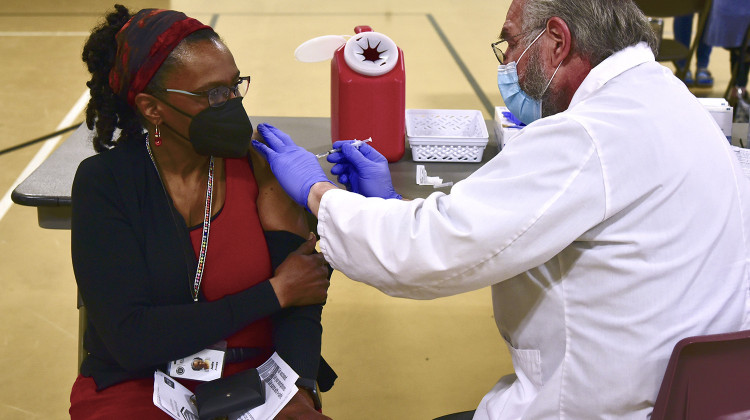
Farah Yousry/Side Effects Public MediaAs healthcare workers in the U.S. received COVID-19 vaccines, many were relieved and hopeful. But doctors who are foreign-born also describe a bittersweet feeling.
Dr. Samuel Urrutia is walking to a coffee shop near University Hospital in Indianapolis. It's freezing but he see it as a good chance to capture videos to share with his parents back in Honduras over the family WhatsApp group.
“My family likes seeing videos of the snow. They've never have actually experienced that. So it's all good,” he says.
Urrutia is a resident in internal medicine at Indiana University. His father is a general practitioner in a rural Honduran village.
“My dad is 57 years old. He is about to retire later this year, actually. But he's still worked through the pandemic because they thought they needed him and he has not received a vaccine,” he says. “There's no plan for mass vaccination in Honduras or even for higher risk population vaccination.”
Honduras is not the only country in this situation. The United Nations says 75 percent of the world’s available vaccines have been administered in only 10 countries. Meanwhile, 130 countries still don’t have a single dose.
Urrutia received the Pfizer vaccine in December — it left him happy and hopeful. But these feelings are tempered when he thinks of family and colleagues back home. “How unfair it is for some people to be seeing 60 or 80 patients a day in a country like Honduras and not be able to access the vaccine."
The global disparity in vaccine access hits home for many doctors serving on the frontline of the pandemic here. Nearly 30 percent of the doctors in the U.S. are foreign-born like Urrutia, mostly from developing countries with limited or no vaccine access.

Dr. Wassim Abdallah, an IU internal medicine resident from Lebanon, says this makes him “angry and sad to see the inequity in vaccine distribution".
“I feel lucky, I was able to get the vaccine, and I'm an immigrant doctor, getting the vaccine even before the President of the United States,” he says. “Whereas like in Lebanon, two months into like the vaccine rollout, so far, nobody has gotten the vaccine inside of the country, including my colleague doctors.”
His grandfather in Lebanon is 102 and has yet to get the vaccine. He worries about his family back home — a lot.
Lebanon received its first batch from the COVID-19 Pfizer-BionTech vaccine doses on Feb. 13, with aid from the World Bank. The country is expected to receive more vaccines throughout the year.
For many developing countries, vaccines are the most effective tool to control the pandemic. COVID lockdowns or even social distancing is hard in places where many rely on daily wages to stay afloat.
John Patton, professor of virology at Indiana University Bloomington, says this allows the virus to spread unchecked. “If you have a population in which the virus is just infecting and spreading, uncontrolled, there is almost a competition among the different viruses that are being produced.”
Patton says this can lead to new virus variants potentially undermining vaccination efforts -- even in countries like the U.S.
Ensuring equitable access to the vaccine is not just “the morally right thing” to do but is in every country’s “pragmatic best interest," says Jennifer Nuzzo, senior scholar at Johns Hopkins Center for Health Security and senior fellow at the Council on Foreign Relations.
“Even if you don't have morals, you do care about, you know, getting to a point where we no longer live in fear of this virus, where we are able to restore economies and lift travel restrictions and go back to the lives that we once enjoyed,” Nuzzo says. “And that requires that all countries have protection.”
Aware of the economic and public health impact of such disparity, the World Health Organization is spearheading a global initiative called COVAX to buy as many as two billion COVID-19 vaccine doses in bulk to ensure wider access.
President Biden announced on Feb. 18 that the U.S. will give $4 billion to COVAX.
Paul Perrin, associate professor of global affairs and global health at the University of Notre Dame, says the will to bridge the gap is important but not enough.
He adds, “Where do you administer these vaccines? Is it in the health system? Well, what if they're people in remote areas? How do they present to the health system?
"And so it's not just as simple as saying, we're going to send vials overseas, and people will be vaccinated. There’s a whole series of steps that need to happen.”
In many developing countries, trust in the government’s ability to deliver a smooth vaccine rollout is limited. This is something Dr. Ahmad Alkashash, a pathology resident at IU, sees in his home country, Egypt.
“The health sector in Egypt is underfunded ... . So I think this is where the problem lies,” he says.
While Egypt managed to secure 40 million doses — enough to vaccinate 20 percent of its population — most healthcare workers remain unvaccinated.

As Alkashash sits in the pathology lab looking in a microscope, he feels lucky to be safe after getting his vaccine last December — and at times guilty too. He says COVID deaths are piling up back home and his doctor friends speak of a thankless situation.
“Every day I log on my Facebook account, every day I see someone who's lost," he says. "That's every day. someone I know. I knew, personally."
This story was produced by Side Effects Public Media, a news collaborative covering public health.
 DONATE
DONATE




 View More Articles
View More Articles

 Support WFYI. We can't do it without you.
Support WFYI. We can't do it without you.